Rural Nursing Workforce
December 2021
by Jessica Rosencrans, BBA and Per Ostmo, MPA
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway disseminates work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. This resource provides a summary of recent research, conducted by the RHRCs, on the rural nursing workforce.
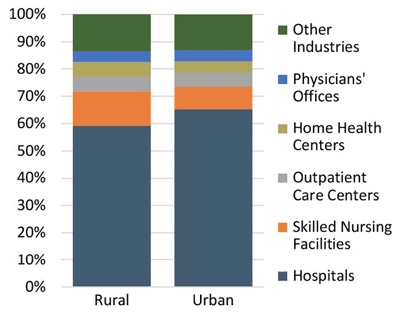
Practice levels for registered nurses (RNs) include Associate of Science in Nursing (ADN), Bachelor of Science in Nursing (BSN), and various advanced practice registered nursing (APRN) degrees, including nurse practitioner (NP). Terminal degrees in the nursing field include Doctorate of Nursing Practice and Doctorate of Philosophy. Nurses play critical roles in numerous practice settings, with hospitals being most common.
Figure 1. Distribution of Nurses Across Principal Employers, 2011 – 2015 American Community Survey1
RN-to-BSN Education Programs
In 2019, more than half of nurses in the U.S. had a bachelor's degree or higher.2 However, the proportion of BSN-prepared nurses decreases as rurality increases.2 Only 46.1% of RNs practicing in rural areas were BSN-prepared versus 57.9% in urban areas.2 In the hospital setting, 50.8% of rural nurses were ADN-prepared versus 38.7% in urban hospitals.1 Despite differences in the educational curriculum between BSN and ADN students, graduates obtaining either degree must pass the same licensing exam.
Due to a relatively high proportion of associate degree RNs in rural areas, RN-to-BSN bridge programs are well-positioned to develop the rural nursing workforce. Most programs can be completed within one year for full-time students or two years for part-time students.2
In a 2018 survey mailed to all RN-to-BSN program directors in the U.S. (N = 758; 247 responses), 55.7% of programs did not offer rural-specific content in their curricula, and only 5.5% offered a specific course in rural health.3 About 38% of programs reported targeting rural students when recruiting, and 58.2% of programs estimated that "less than 25%" of students were from rural areas.3 For comparison, 54% of NP programs reported actively recruiting students from rural areas.2
The top five potential barriers to recruiting students to RN-to-BSN programs, regardless of rurality, were:
- Family obligations of prospective students (73.0% of respondents)
- Work obligations of prospective students (72.2%)
- Cost of tuition (56.5%)
- Required non-nursing courses (46.0%)
- Lack of tuition reimbursement by employers (42.2%)3
Rural-relevant issues for online learners included lack of information technology assistance, and internet accessibility and affordability.2
Nurse Practitioners as Primary Care Providers
Between 2010 and 2016, the NP workforce in the U.S. grew at an annual rate of 9.4%, while the overall physician workforce grew at 1.1%.4 NPs currently represent one in five primary care clinicians and have become an integral part of the primary care workforce, particularly in rural areas.5 Forty percent of rural primary care practices employ at least one NP versus 26.5% of urban practices.5 Additionally, a greater share of NPs than physicians practice in rural areas (21% of all NPs versus 12% of all primary care physicians).5
Job Preparedness
In a 2018 survey of RNs and APRNs, 6.9% indicated that their education did not prepare them for work. 6A higher percentage of nurses living in rural areas reported feeling ill-prepared (15.3%) compared with suburban (5.1%) and urban (5.4%) nurses.6 Male nurses and those who did not report their gender were more likely to report feeling ill-prepared than female nurses (19.6% versus 5.4%).6
Additionally, rural patients are more likely to have multiple chronic conditions and a higher prevalence of poor health-related behaviors, which may result in more complex health care needs than non-rural patients and affect feelings of job preparedness among nurses.6
Job Satisfaction
Of 435 nurses surveyed across all levels of education, most indicated they were satisfied with their profession and jobs, with no difference based on practice location.7 Most nurses reported that it was "not at all likely" that they would leave nursing (94.2%) or their current job (73.3%) within the next year.7
Perceived barriers to nursing practice can impact job satisfaction. The top three barriers reported to occur at least weekly were:
- Too much work to do well (40.7% of respondents)
- Organizational rules and procedures (28.7%)
- Lack of equipment/supplies (18.5%)7
Regardless of rural/urban status, nurses expressed high satisfaction with their perceived ability to use personal initiative or judgment, but lower levels of satisfaction with administrative support.7
Rural Challenges
Among ADNs and BSNs, rural ADN-prepared nurses in physicians' offices had the lowest average annual salary ($37,273) while urban, BSN-prepared nurses in hospitals had the highest ($61,406).1 There is a roughly $8,000 annual salary difference between ADNs and BSNs in rural hospital or skilled nursing facility settings.1 Urban nurses, on average, earn nearly $4,500 more per year than rural nurses.1
A higher proportion of nurses in rural settings (62.0%) were dissatisfied with paperwork than nurses in urban settings (39.8%).7 Nurses in rural areas report higher patient-to-nurse caseloads than in urban areas and are often under-resourced.2 Rural nurses may also experience more interpersonal stressors due to their connections to their communities while simultaneously experiencing increased professional isolation.2
Conclusions
Emphasizing practice autonomy may be a successful strategy when recruiting NPs to rural areas.5 Partnerships between community colleges and local healthcare organizations may help decrease the rural-urban BSN disparity, since these programs are cost-effective and broadly available in rural areas.2 Lastly, the salary difference between rural ADNs and BSNs may encourage higher educational attainment if jobs are available in their communities.1
Resources
- Rural and Minority Health Research Center (2019). Rural Registered Nurses: Educational Preparation, Workplace, and Salary.
- Rural and Minority Health Research Center (2020). A National Survey of RN-to-BSN Programs? Are They Reaching Rural Students?
- Rural and Minority Health Research Center (2019). RN-to-BSN Programs: Challenges for Rural Nurse Education.
- WWAMI Rural Health Research Center (2020). Supply and Distribution of the Primary Care Workforce in Rural America: 2019.
- University of Minnesota Rural Health Research Center (2020). Nurse Practitioner Autonomy and Complexity of Care in Rural Primary Care.
- Rural and Minority Health Research Center (2020). Factors Associated with Perceived Job Preparedness Among RNs: Results From a National Survey.
- Rural and Minority Health Research Center (2019). Perceived Facilitators and Barriers to Rural Nursing Practice.
