Rural Hospital Closures: 2023 Update
June 2023
by Per Ostmo, MPA
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway disseminates work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. This resource provides a summary of recent research, conducted by the RHRCs, on rural hospitals.
Hospital Type and Location
As of December 2020, there were 4,306 acute hospitals in the U.S., comprised of 1,334 Critical Access Hospitals (CAHs), 11 cancer hospitals, 1,924 Prospective Payment System hospitals (PPS-only), and 1,037 PPS hospitals with special payment designations.1 See Figure 1. There were 2,176 acute hospitals in rural locations and 2,130 in urban locations.1
Counties with a population of 50,000 or less were primarily served by CAHs while counties with more than 50,000 residents were primarily served by PPS hospitals.1 While CAHs are typically located in rural areas, a CAH may be located in an urban county and reclassify as rural under certain conditions.2 The acute average daily census (ADC) in hospitals in counties with a population of 50,000 or less was much lower than in hospitals in counties with a population greater than 50,000.1 Furthermore, CAHs had lower median acute ADCs than PPS hospitals across all sizes of counties.1
Figure 1. Number of Acute Hospitals by Type and Location, 20201

Rural Hospital Closures
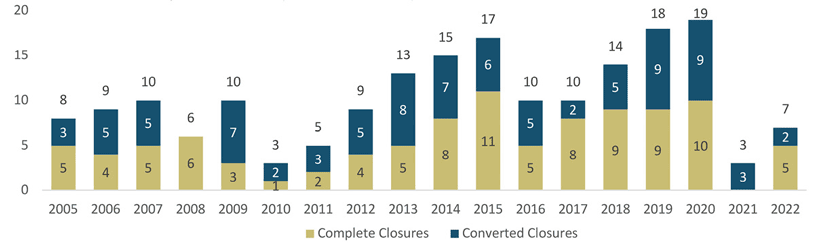
Hospital closures are categorized as "complete" closures, where facilities no longer provide any health care services, or "converted" closures, where facilities no longer provide in-patient care, but continue to provide some health care services.3 From 2005 through 2022, 186 rural hospitals closed (100 complete, 86 converted).3 See Figures 2 and 3.
These closures have been comprised of:
- 75 PPS hospitals
- 65 CAHs
- 30 Medicare Dependent Hospitals
- 12 Sole Community Hospitals
- 3 Indian Health Service hospitals
- 1 Rural Referral Center1,3
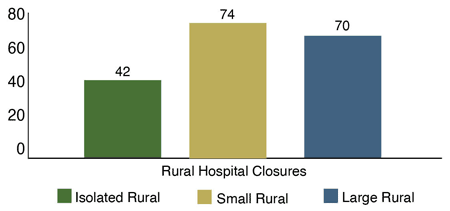
Of the 186 closures from 2005 through 2022, most have been located in small rural areas, followed by large rural areas, then isolated rural areas.3 See Figure 2.
Figure 2. Rural Hospital Closures by Rurality, 2005-20223
Between 1990 and 2020, rural counties that experienced a within-county hospital closure became more economically unequal, with higher unemployment, lower per capita income, and lower median household incomes compared with rural counties overall.4 These rural closure counties were also increasingly likely to be primary care and dental care health professional shortage areas prior to hospital closure.4 Furthermore, closure counties have had increasing shares of non-White residents, suggesting a more racially disparate impact.4 The median proportions of Black, Hispanic, and American Indian residents in counties with rural hospital closures were higher than the medians in rural counties overall.4 In the 2010s, two-thirds of all rural closures nationally were in the South, home to over half of Black people in the U.S., and where most states have not expanded Medicaid.4
Figure 3. Rural Hospital Closures: Complete Versus Converted 2005-20223
Service Provision in Rural Hospitals
From 2009 to 2017, the percentage of hospitals offering birthing/postpartum services, medical/surgical intensive care, obstetrics, and skilled nursing declined in both rural CAHs and rural PPS hospitals.5 Additionally, rural CAHs became less likely to offer adult general medicine/surgery and home health services while rural PPS hospitals became less likely to offer pediatric general medicine/surgery.5
Similarly, from 2011-2017, the availability of obstetric services and skilled nursing services decreased among hospitals in nonmetropolitan counties with a greater percentage of residents belonging to an Agency for Healthcare Research and Quality (AHRQ)-identified priority population (Hispanic/Latino population, non-Hispanic Black population, population aged 65 years or older, and population in poverty).6 Conversely, the availability of oncology services, hospital-based outpatient services, orthopedic services, and emergency psychiatric services increased in nonmetropolitan counties with a greater percentage of residents belonging to AHRQ priority populations.6
Revenue and Profitability of Rural Hospitals
Between 2017 and 2020, compared with rural hospitals that remained open, most rural hospitals that closed were much more unprofitable and much less liquid.7 Operating margin measures the profit a hospital makes on a dollar of revenue from patient care, while total margin measures the profit a hospital makes on a dollar of revenue from patient care and all other activities. Days cash on hand measures how long a hospital can continue to pay its operating expenses with the current cash it has available. Among 56 rural hospital closures between 2017 and 2020, in the year before closure, 49 had a negative operating margin, 50 had a negative total margin, and 47 had less than 30 days cash on hand.7
From 2011 to 2019, after adjusting for inflation, total outpatient revenue for the average rural hospital increased by 56.4% while total inpatient revenue increased by only 9.3%.8 In 2019, the typical rural hospital received nearly three-fourths of its revenue from outpatient services, with inpatient services comprising an increasingly smaller percentage of patient revenue since 2011.8
Resources
- North Carolina Rural Health Research and Policy Analysis Center (2022). Types of Rural and Urban Hospitals and Counties Where They Are Located.
- Rural Health Information Hub (Accessed January 2023). Critical Access Hospitals landing page.
- The Cecil G. Sheps Center for Health Services Research (Accessed January 2023). Rural Hospital Closures landing page.
- North Carolina Rural Health Research and Policy Analysis Center (2022). Since 1990, Rural Hospital Closures Have Increasingly Occurred in Counties That Are More Urbanized, Diverse, and Economically Unequal.
- North Carolina Rural Health Research and Policy Analysis Center (2022). Changes in the Provision of Health Care Services by Rural Critical Access Hospitals and Prospective Payment System Hospitals in 2009 Compared to 2017.
- North Carolina Rural Health Research and Policy Analysis Center (2022). Association Between Rural Hospital Service Changes and Community Demographics.
- North Carolina Rural Health Research and Policy Analysis Center (2022). Rural Hospitals That Closed Between 2017‐20: Profitability and Liquidity in the Year Before Closure.
- North Carolina Rural Health Research and Policy Analysis Center (2022). Trends in Revenue Sources Among Rural Hospitals.
