Quality Star Ratings: Hospitals, Skilled Nursing Facilities, and Home Health Agencies
March 2024
by Per Ostmo, MPA
Funded by the Federal Office of Rural Health Policy (FORHP) within the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway disseminates work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. This resource provides a summary of recent research, conducted by the RHRCs, on quality star ratings.
Overall Hospital Quality Star Ratings
The Centers for Medicare & Medicaid Services (CMS) Overall Hospital Quality Star Rating system summarizes a variety of measures across areas of quality into a single star rating for each hospital, with more stars indicating higher quality.1 The 2022 Overall Hospital Quality Star Rating selects 46 measures and categorizes them into five groups: mortality, safety of care, readmission, patient experience, and timely and effective care.1 To be eligible to receive a star rating, three measures in three measure groups must be present, one of which must be mortality or safety of care.1 The Overall Hospital Quality Star Rating for July 2022 public reporting was calculated using July 2021 Care Compare data and included 4,489 hospitals—3,121 of which met reporting criteria.1 See Table 1.
Table 1. National Distribution of Overall Hospital Quality Star Ratings, July 20221
| Overall Rating | Number of Hospitals (N=4,489, %) |
|---|---|
|
|
198 (4.4%) |
|
|
702 (15.6%) |
|
|
895 (19.9%) |
|
|
895 (19.9%) |
|
|
431 (9.6%) |
| N/A | 1,368 (30.5%) |
In addition to helping patients decide where to receive services and encouraging hospitals to improve the quality of services provided, star ratings are also used in reimbursement contracts that hospitals negotiate with insurance companies.2 However, many rural hospitals do not have a CMS Overall Hospital Quality Star Rating because of an insufficient number of hospital cases, hospital decisions to not participate, and CMS data requirements (rural hospitals may not provide the services that are measured by CMS quality reporting programs).2 Furthermore, some CMS quality initiatives systematically exclude some rural hospitals from participation because they are paid differently than other providers.2 The absence of a star rating may be misinterpreted by patients as an indicator of low-quality care and may impede hospitals' ability to negotiate contracts with partners.2
Rural Versus Urban Hospitals
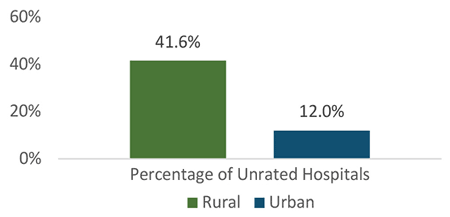
An analysis of 2016 and 2021 CMS Hospital Quality Star Ratings and 2019 Medicare cost report data from the Healthcare Cost Report Information System revealed several disparities between rural and urban hospitals.2 The final dataset included 4,511 hospitals, with 2,173 classified as rural.2 First, a much higher percentage of rural hospitals were unrated compared to urban hospitals. In 2021, 41.6% of rural hospitals (n=903) were unrated compared to only 12.0% of urban hospitals (n=280).2 See Figure 1. Among unrated hospitals, 76.3% were rural and 23.7% were urban.2
Figure 1. Percentage of Hospitals Without a CMS Hospital Quality Star Rating, 20212
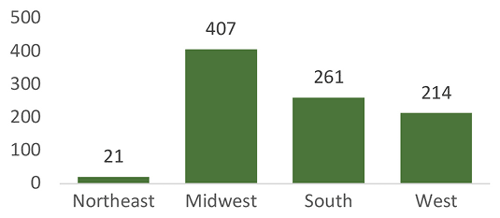
Second, there was a large increase in the percentage of unrated rural hospitals between 2016 (34.3%, n=762) and 2021 (41.6%, n=903).2 Additionally, a wider range of star ratings emerged among rural hospitals. By 2021, rural hospitals were more likely to have 1 star (2.1%) or 5 stars (7.2%) than they were in 2016 (0.4% and 0.7%, respectively).2 Third, almost all unrated rural hospitals were Critical Access Hospitals (CAHs). In 2021, 807 CAHs were unrated compared to 686 in 2016.2 Fourth, most unrated rural hospitals had net patient revenue less than $20 million (a proxy for hospital size). In 2021, the number of unrated rural hospitals with net patient revenue less than $20 million was 605, compared to 629 in 2016.2 Fifth, almost half of unrated rural hospitals were in the Midwest census region. In 2021, 407 rural hospitals in the Midwest were unrated compared to 223 in 2016.2 See Figure 2.
Figure 2. Number of Rural Hospitals Without a CMS Hospital Quality Star Rating by Census Region, 20212
Skilled Nursing Facilities
A separate study examined quality among skilled nursing facilities (SNFs) serving rural Medicare beneficiaries using the 2018 Nursing Home Compare Provider File and the 2018 Post-Acute Care and Hospice Utilization and Payment Public Use File (PAC PUF).3 There were five categories of SNF by rurality: (1) non-rural-serving urban SNF (serving fewer than 10% rural beneficiaries), (2) rural-serving urban SNF (serving 10% or more rural beneficiaries), (3) SNF located in large rural community, (4) SNF located in small rural community, and (5) SNF located in isolated small rural community.3 Of the 15,230 Medicare-certified SNFs operating in 2018, 14,685 were eligible for analysis, with 28.7% located in rural communities and 71.3% located in urban communities.3 Of the urban SNFs, 23.4% were rural- serving.3
Nursing Home Compare uses three sub-ratings to determine the overall star rating: quality star rating, survey star rating, and staffing star rating.3 The quality star rating is derived from 15 resident-level clinical measures.3 The survey star rating is based on annual health and safety inspections to examine compliance with Medicare and Medicaid regulations.3 The staffing star rating is based on the ratio of nurse staffing hours per resident per day.3
While rural-serving status was not significantly associated with overall or staffing star ratings, significant variation was found in both quality and survey star ratings.3 Compared to non-rural-serving urban SNFs, rural-serving urban SNFs were 34% less likely to have high quality star ratings, and SNFs located in large rural, small rural, and isolated small rural communities were 44%, 41%, and 25% less likely to have high quality star ratings, respectively.3 SNFs located in isolated small rural communities were 33% more likely to have high survey star ratings compared to non-rural-serving urban SNFs.3
Home Health Agencies
A companion study used 2018 Home Health Compare Provider File and 2018 PAC PUF data to examine quality among home health agencies (HHAs) serving rural Medicare beneficiaries.4 There are two star ratings for HHAs reported on Home Health Compare: quality of patient care and patient experience.4
There were approximately 11,500 HHAs active at some point during 2018.4 A total of 8,304 HHAs were eligible for the quality of patient care analysis.4 Of these, 18.5% were located in rural communities and 81.5% were located in urban communities.4 Of the urban HHAs, 22.0% were rural-serving.4 A total of 5,494 HHAs were eligible for the patient experience analysis.4 Of these, 22.8% were in rural communities and 77.2% were in urban communities.4 Of the urban HHAs, 28.8% were rural-serving.4
Rural-serving urban HHAs were nearly twice as likely to have high patient experience star ratings compared to non-rural-serving HHAs.4 HHAs located in large, small, and isolated small rural communities were even more likely to have high patient experience star ratings compared to non-rural-serving urban HHAs, with the likelihood of high ratings increasing with rurality.4 HHAs in isolated small rural communities were four times as likely to have high patient experience star ratings than non-rural-serving urban HHAs.4 It is possible the higher patient experience ratings in rural communities reflect a greater feeling of community among HHA staff and beneficiaries.4 Quality of patient care star ratings were not significantly associated with rural- serving status.4
Resources
- Yale New Haven Health Services Corporation (2022). Overall Hospital Quality Star Rating on Care Compare: July 2022 Updates and Specifications Report.
- North Carolina Rural Health Research and Policy Analysis Center (2021). 2021 CMS Hospital Quality Star Ratings of Rural Hospitals.
- WWAMI Rural Health Research Center (2022). Quality of Skilled Nursing Facilities Serving Rural Medicare Beneficiaries.
- WWAMI Rural Health Research Center (2022). Quality of Home Health Agencies Serving Rural Medicare Beneficiaries.
