Quality of Care in Rural Hospitals
January 2019
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. The RHRCs are committed to providing timely, quality research on the most pressing rural health issues. This resource provides a summary of recent research on quality of care.
As healthcare payment models shift from patient volume to value-based care, there has been a push for higher quality healthcare services at lower cost. The National Quality Strategy uses various methods to assess and improve quality including a shift from a fee-for-service model to pay-for-performance.1 Reimbursement for care is now contingent upon the quality of the healthcare provided and patient outcomes. However, developing these measures across unique health systems has been difficult, especially for low patient volume rural providers. Tracking relevant quality measures for each Critical Access Hospital (CAH) in a network or health system could improve both the quality of rural healthcare and reimbursement for rural providers.2
Collection of Rural Quality Measures
Currently, the Centers for Medicare & Medicaid Services (CMS) employ Star Quality Ratings for hospitals. Although well recognized as a healthcare quality measurement system for Medicare Advantage contracts, some stakeholders argue that it is not an effective quality measure for hospitals and excludes many small rural hospitals.3 Under this system, hospitals are ranked utilizing self-reported data on 64 measures. Many small and rural hospitals do not have the patient volumes or specific services that are measured and evaluated as part of the Star Quality Ratings.3
In 2017, 34% of all rural hospitals, including CAHs and Prospective Payment System (PPS) hospitals, were not rated under the CMS Star Quality Rating compared to only 12% of urban hospitals.3 See Table 1. When hospitals are excluded and do not receive a rating, individuals who review the quality of their local hospital(s) may equate no rating with poor quality care or simply negligence in reporting, even though CMS states this is not the case.
Table 1. CMS Star Categories 20173
| Star Quality Rating | Rural | Urban | Total |
|---|---|---|---|
|
|
8 (7%) | 99 (93%) | 107 |
|
|
166 (25%) | 502 (75%) | 668 |
|
|
848 (48%) | 915 (52%) | 1,763 |
|
|
422 (45%) | 517 (55%) | 939 |
|
|
15 (18%) | 67 (82%) | 82 |
| Not Rated | 762 (73%) | 286 (27%) | 1,048 |
| Total Hospitals | 2,221 | 2,386 | 4,607 |
Small rural hospitals were less likely than large rural hospitals to receive a star rating, and 43% of those not rated were located in the Midwest census region.3 The missing data limits the conclusions that can be drawn from these hospital comparisons. Due to the exclusion of hospitals in the CMS rating, some rural hospitals continue to look for other avenues to report on quality including through the Medicare Beneficiary Quality Improvement Program (MBQIP).3
Quality of Rural Healthcare
There is no consensus on which measures are clear indications of quality healthcare. Given variability in the definition of "quality healthcare services," research also reports variable quality among rural health services. In rural areas:
- Rural counties report poorer scores than urban counties on preventable hospitalizations (71.4 per 100,000 vs. 56.1 urban), receiving HbA1c monitoring (0.84 vs. 0.86), and receiving mammography screening (0.59 for rural vs. 0.62 among urban).4
- Rural hospitals report less post-hospital discharge follow-up care among Medicare beneficiaries (0.81 among rural vs. 0.92).5
- Emergency rooms in small rural or isolated small rural area hospitals saw a higher percentage (67%) of patients with non-emergent conditions compared to urban hospitals (62.2%).6
Although rural hospitals did not perform as well on preventable hospitalizations, certain screenings, and posthospitalization follow-up care, CAHs do report having fewer adverse drug events (ADEs) among the top four ADEs (55.9 per 100,000).4,5 Rural PPS hospitals reported 76.2 per 100,000 for the top four ADEs and urban hospitals reported 67.2 per 10,000 for the top four ADEs.7
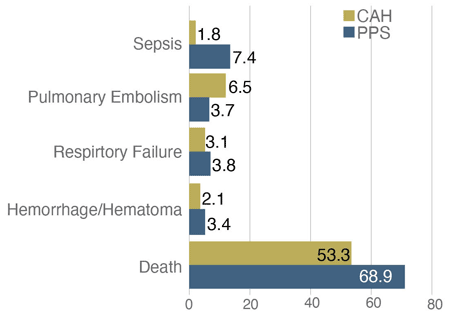
There have also been improvements in care quality for rural hospital-based nursing homes. From 2006-2011, the rural hospital-based nursing homes reported a 56% decrease in the use of physical restraints and a 16% decrease in the long-stay composite measure.8 CAHs also provide high-quality surgical care on par with larger rural and urban PPS hospitals of comparable size.9 See Figure 1. On average, CAHs had fewer cases of perioperative hemorrhage or hematoma, perioperative pulmonary embolism or deep vein thrombosis, and postoperative sepsis.9
Figure 1. Surgical Patient Outcome Measures9
Future of Rural Hospital Quality
With the movement towards pay-for-performance, more rural hospitals are working to identify new and relevant quality measures that can demonstrate the quality of care being provided in a rural setting. As an example, rural CAHs are working on reporting measures that illustrate the quality and efficacy of swing-beds in rural communities.2
Some of the quality measures that CAHs and CAH networks have begun measuring include:
- Discharge disposition
- Average length of stay
- Readmission within 30 days
- Functional status
- Process of care
- Patient experience of care
The goals of creating these quality measures are to improve care and to be able to compare rural quality of care to other post-acute care providers. However, some of the challenges that CAHs face in implementing these quality measures and collecting data include limited staff, limited resources, and the difficulty of analyzing inpatient and swing-bed patient data separately.2
Resources
- University of Minnesota Rural Health Research Center (2015). Rural Hospital and Physician Participation in Private Sector Quality Initiatives.
- University of Minnesota Rural Health Research Center (2018). Critical Access Hospital Swing-Bed Quality Measures: Findings From Key Informant Interviews.
- North Carolina Rural Health Research and Policy Analysis Center (2017). CMS Hospital Quality Star Rating: For 762 Rural Hospitals, No Stars Is the Problem.
- University of Minnesota Rural Health Research Center (2017). Rural-Urban Differences in Medicare Quality Scores Persist After Adjusting for Sociodemographic and Environmental Characteristics.
- North Carolina Rural Health Research and Policy Analysis Center (2015). Rural Medicare Beneficiaries Have Fewer Follow-Up Visits and Greater Emergency Department Use Post Discharge.
- North Dakota and NORC Rural Health Reform Policy Research Center (2015). Use and Performance Variations in U.S. Rural Emergency Departments: Implications for Improving Care Quality and Reducing Costs.
- University of Minnesota Rural Health Research Center (2017). Identifying Adverse Drug Events in Rural Hospitals: An Eight-State Study.
- University of Minnesota Rural Health Research Center (2015). Nurse Staffing Levels and Quality of Care in Rural Nursing Homes.
- RUPRI Center for Rural Health Policy Analysis (2016). Surgical Patient Safety Outcomes and CAHs: How Do They Compare?
