Rural Obstetric Services: Access, Workforce, and Impact
April 2019
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. The RHRCs are committed to providing timely, quality research on the most pressing rural health issues. This resource provides a summary of some of their recent research.
Access to Care
Pregnant women who have access to quality obstetric (OB) care have better maternal and child health outcomes. However, ensuring access for rural women has become problematic. Between 2004 and 2014, 179 rural counties lost hospital-based OB services.1,2 As a result of OB unit and hospital closures, by 2014:
- 54% of rural counties lacked hospital-based OB services (up from 45% in 2004).1
- Only 30% of rural noncore counties had in-county, hospital-based OB care compared to 78% of micropolitan counties.1
- More than half of rural counties had no hospital-based OB services.2,3
- The most rural areas (noncore counties) had fewer hospitals providing OB care and experienced the greatest reduction in services.1
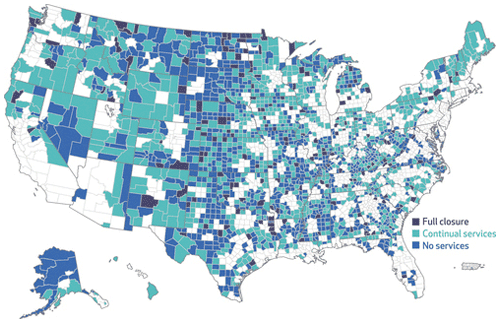
Availability of hospital-based OB services in 2014 also varied by state. For example, more than two-thirds of rural counties in Florida (78%) reported no in-county hospital OB services compared to only 9% of rural counties in Vermont.4 See Figure 1.
Counties with greater odds of having no hospital-based OB services in 2014 were those with:
- Fewer OBs per women of reproductive age
- Fewer family physicians (FP) per capita
- Lower birthrates
- A higher percentage of non-Hispanic Black women of reproductive age
- Lower median household incomes
- More restrictive Medicaid income eligibility thresholds.2,3
Similarly, factors associated with a rural OB unit closure included a limited supply of OBs and/or FPs, private hospital ownership, being located in a lower income community, and smaller hospital size.5 Discontinuation of OB services was also more likely among critical access hospitals (CAHs) than other rural hospitals.5 However, this particular study found closures were not related to system affiliation, distance to the nearest hospital providing OB services, or the proportion of women reporting Medicaid as their primary payer.5
Figure 1. Hospital Obstetric Services in Rural Counties, 2004 – 20143
Rural Obstetric Workforce
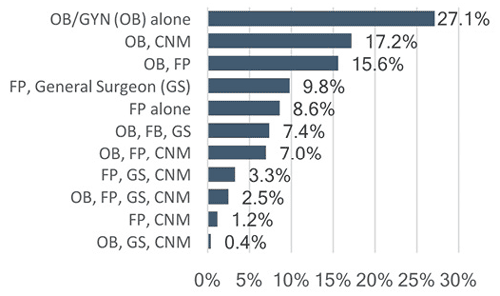
Research on both availability of hospital OB services and factors associated with OB unit closures identifies OB and FP workforce shortages as a primary concern. It also indicates that smaller rural hospitals rely more heavily on FPs to provide OB care.1-3,5 In a 2013-14, nine-state survey of rural hospitals providing obstetric services, researchers found that 77% had OBs attending deliveries.6 Additionally, more than half (55.3%) reported FPs doing deliveries, 32% had FPs performing cesareans, 31.6% indicated certified nurse midwives (CNMs) attended deliveries, and 23.4% relied on general surgeons to perform cesarean deliveries.7 See Figure 2.
Figure 2. Percentage of Rural Hospitals by Type(s) of Clinicians Attending Deliveries, 2013‑147
Nearly all of the 238 surveyed rural hospitals (98%) identified challenges in staffing OB units. The primary challenge (reported by 36% of rural hospitals) related to scheduling. This included scheduling OB nurses, dealing with vacation, sick, medical, maternity leaves, covering night shifts/weekends, and getting nurses to be on call and/or to come in when needed. Training was a challenge for 23% of respondents. Specifically, access to training, maintaining nurse competencies in low birth volume settings, and a need to cross-train nurses for OB and other areas of the hospital. Recruiting and retaining qualified physicians or nurses was a concern for 20.6% of rural hospitals. Similarly, 19.8% reported issues of census fluctuation to include both concern around having enough nurses when census is high, and also having nurses on unit during low census. Finally, 11.9% reported intra-hospital relationships as a significant concern noting that others do not understand the high-risk nature of OB or why it is difficult to follow guidelines and meet productivity standards. There is also difficulty justifying OB nurse staffing to administration when census is low.6,8
Impact of Limited Access to OB Services
Compared to rural counties with continual OB services, loss of services in rural counties not adjacent to urban areas was associated with significant increases in:
- Out-of-hospital births
- Births in a hospital without an OB unit
- Preterm births9
Loss of hospital-based OB services among rural counties that were adjacent to urban areas was associated with low prenatal care use and an increase in births in hospitals without OB services although this gap declined over time.9
Conclusions
The number of counties with hospital-based OB services continues to decline with greater reduction in services in rural and noncore counties. Additionally, counties that are more likely to experience closure of an OB unit or to report no OB services, are in states with restrictive Medicaid income eligibility thresholds or those that serve greater percentages of women who are non-Hispanic Black or lower income, all of which creates a greater disparity for at-risk women in rural areas. Limited rural access results in more out-of-hospital births, births in hospitals with no OB services, and preterm births.
There is need for interprofessional education;7 training for staff in low-volume hospitals, especially on obstetric emergencies;6,7 and development of innovative care models that propose regionalization of care, partnerships with larger health systems, and/or the use of telehealth services.9 Community, clinical, and policy efforts to support rural maternity care access, especially in places without hospital-based OB services, may include training first responders in emergency OB care, providing transportation or housing support for rural residents who travel for OB care, and community-based pregnancy, breastfeeding, and parenting supports.
Resources
- University of Minnesota Rural Health Research Center (2017). Closure of Hospital Obstetric Services Disproportionately Affects Less-Populated Counties.
- University of Minnesota Rural Health Research Center (2018). Association Between Loss of Hospital-Based Obstetric Services and Birth Outcomes in Rural Counties in the United States. JAMA, 319(12):1239-1247.
- University of Minnesota Rural Health Research Center (2017). Access to Obstetric Services in Rural Counties Still Declining, With 9 Percent Losing Services, 2004-14. Health Affairs, 36(9), 1663-1671.
- University of Minnesota Rural Health Research Center (2017). State Variability in Access to Hospital-Based Obstetric Services in Rural US Counties.
- University of Minnesota Rural Health Research Center (2016). Why Are Obstetric Units in Rural Hospitals Closing Their Doors? HSR, 51(4): 1546-60.
- University of Minnesota Rural Health Research Center (2015). The Rural Obstetric Workforce in US Hospitals: Challenges and Opportunities. JRH, 31(4): 365-72.
- University of Minnesota Rural Health Research Center (2014). The Obstetric Care Workforce in Critical Access Hospitals (CAHs) and Rural Non-CAHs.
- University of Minnesota Rural Health Research Center (2017). The Maternity Care Nurse Workforce in Rural U.S. Hospitals. J Obstet Gynecol Neonatal Nurs, 46(3):411-22.
- University of Minnesota Rural Health Research Center (2018). Association Between Loss of Hospital-Based Obstetric Services and Birth Outcomes in Rural Counties in the United States. JAMA, 319(12): 1239-47.
