Rural Behavioral Health
November 2017
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) with diverse audiences. The RHRCs are committed to providing timely, quality national research on the most pressing rural health issues. This resource provides a summary of their most recent research on behavioral health.
Prevalence
Any mental illness is any diagnosable mental, behavioral, or emotional illness other than substance use.1 During 2015, roughly 43.4 million adults in the U.S. had some kind of mental illness.2 During 2010-2011, nonmetropolitan counties reported a higher percentage of residents with any mental illness (19.5%) than metropolitan counties (17.8%).3 The highest rate of any mental illness (22.5%) occurred among rural residents in the western U.S. region.3
Nationally, 4% reported a serious mental illness, though rates rose with increasing rurality.3 Rural micropolitan residents in the western U.S. region reported the highest percentage of serious mental illness (6.8%).3 The lowest rate occurred in large central counties in the southern region of the U.S. (2.7%).3
Adverse Childhood Experiences
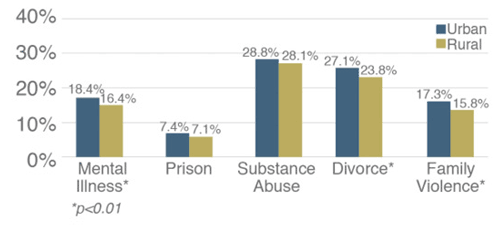
Adverse childhood experiences (ACEs) are occurrences in family relationships that prevent children from finding the support and safety they need for healthy growth.4 The more ACEs, the higher the risk for behavioral and physical health problems in adulthood.4 More than half (56.5%) of rural residents had been exposed to some form of ACE during 2011-2013.4 See Figure 1.
Figure 1. Prevalence of ACE Types in Rural and Urban Adults: Household Dysfunction4
Access to Behavioral Health Care
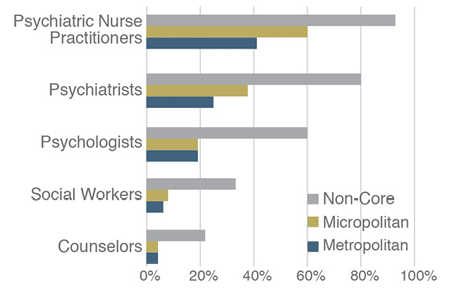
As of October 2015, rural communities reported a smaller proportion of behavioral healthcare providers than urban areas, including fewer psychiatrists, clinical psychologists, psychiatric nurse practitioners, social workers, and counselors.5 See Table 1 and Figure 2.
Table 1. Behavioral Health Providers per 100,000 Population in U.S. Counties5
| Provider | Metropolitan | Micropolitan | Non-Core |
|---|---|---|---|
| Counselors | 118.10 | 100.20 | 67.10 |
| Social Workers | 66.40 | 45.00 | 29.90 |
| Psychologists | 33.20 | 16.80 | 9.10 |
| Psychiatrists | 17.50 | 7.50 | 3.40 |
| Psychiatric Nurse Practitioners | 2.20 | 2.10 | 0.90 |
Figure 2. Percent of U.S. Counties Without Behavioral Health Providers5
Fewer providers may lead to increased utilization of the emergency department (ED) for mental health and substance abuse (MH/SA) treatment.
- Overall in 2013, 14.6% of all ED visits were for a primary MH/SA diagnosis.6
- Large rural (58.4%), small rural (62.3%), and isolated small rural (62.1%) residents presenting to the ED with a primary MH/SA diagnosis were more likely to be on public insurance than urban residents (48.0%).6
- Among urban MH/SA ED patients, 18.2% were 65 years of age and older compared to 22.3%, 26.4%, and 27.9% of large rural, small rural, and isolated small rural, respectively.6
Though related to substance abuse, 2016 data indicated a disparity in rural access to buprenorphine-naloxone prescribers as well. Buprenorphine-naloxone is an effective treatment for opioid use disorder.7 Roughly half (52.5%) of all counties had at least one physician with a Drug Enforcement Agency waiver to prescribe buprenorphine in 2016.7 Urban counties were more likely than rural to have access to waivered providers; 65.9% of metropolitan counties had at least one provider compared to 45.4%, 59.5%, and 23.8% of adjacent to metropolitan, micropolitan not adjacent to metropolitan, and small and remote rural counties, respectively.7
Rural Behavioral Health Interventions
Mental Health First Aid
Mental Health First Aid (MHFA) training is an early intervention program aimed at improving population level behavioral health treatment-seeking.8 MHFA rural graduates indicated confidence in their mastery of MHFA. However, given the primary focus of MHFA is to encourage treatment-seeking, rural communities may not have the workforce to meet the demands of those who would then seek treatment.8
Telemental Health
Telemental health refers to providing mental healthcare from one site to another using electronic technology. This intervention can address the most basic hurdles to rural mental healthcare, including shortages of mental health clinicians and extended travel distances.9 Quality telemental health access in rural areas has grown while the cost has decreased. However, the fee-for-service reimbursement model does not provide sufficient financial reimbursement or incentive to sustain growth. Growth in telemental health is also burdened by workforce supply challenges, issues with recruitment and retention, and high rates of un-insurance and under-insurance in rural areas.9 To expand rural access to telemental health, issues regarding reimbursement, administration, and provider supply must be addressed.9
Conclusion
Rural communities report a higher proportion of the population with mental illness, serious mental illness, and substance use. Rural behavioral health issues are compounded by a lack of access to care. Rural solutions need adequate reimbursement and must be sustainable when treating the uninsured and under-insured.
Resources
- SAMHSA. (2013). The NSDUH Report. Rockville, MD: U.S. Department of Health and Human Services.
- Center for Behavioral Health Statistics and Quality. (2016). 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51).
- Rural Health Reform Policy Research Center (2014). The 2014 Update of the Rural-Urban Chartbook.
- Maine Rural Health Research Center (2016). Adverse Childhood Experiences in Rural and Urban Contexts.
- WWAMI Rural Health Research Center (2016). Supply and Distribution of the Behavioral Health Workforce in Rural America.
- Rural Health Reform Policy Research Center (2017). Rural and Urban Utilization of the Emergency Department for Mental Health and Substance Abuse.
- WWAMI Rural Health Research Center (2017). Changes in the Supply of Physicians with a DEA DATA Waiver to Prescribe Buprenorphine for Opioid Use Disorder.
- Maine Rural Health Research Center. Talbot J.A., Ziller E.C., & Szlosek D.A. (2016). Mental Health First Aid in Rural Communities: Appropriateness and Outcomes. JRH, 33(1), 82-91.
- Maine Rural Health Research Center. Lambert D., Gale J., Hartley D., Croll Z., & Hansen A. (2016). Understanding the Business Case for Telemental Health in Rural Communities. J Behav Health Serv Res, 43(3), 366-379.
