LGBTQ+ Health: Rural vs Urban Inequities
March 2024
by Jessica Rosencrans, BBA
Funded by the Federal Office of Rural Health Policy (FORHP) within the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway disseminates work of the FORHP-funded Rural Health Research Centers (RHRCs). This resource provides a summary of recent research, conducted by the University of Minnesota RHRC, on the health of rural LGBTQ+ individuals.
Self-Rated Health and Chronic Conditions
From 2019-2020, rural lesbian, gay, and bisexual (LGB) adults were more likely to report poor/fair self-rated health than rural heterosexual adults.1 When adjusting for age, sex, race, ethnicity, educational attainment, and income, rural LGB adults had lower likelihood of excellent/very good/good self-rated health than rural heterosexual adults.1
Prevalence of chronic conditions, including arthritis, asthma, cancer, coronary heart disease, high cholesterol, depression, anxiety, diabetes, heart attack, hypertension, stroke, and chronic obstructive pulmonary disorder, were examined in rural LGB residents from 2019-2020.2
By both rurality and sexual orientation, rural LGB adults were found to be the most likely to report having three or more chronic conditions (44%) and the least likely to report having zero chronic conditions (19%).2 Alternatively, urban heterosexual adults were the most likely to have zero chronic conditions (39%) and the least likely to have three or more chronic conditions (23%).2 See Figure 1.
Figure 1. Number of Chronic Conditions by Sexual Orientation and Rurality, 2019-20202
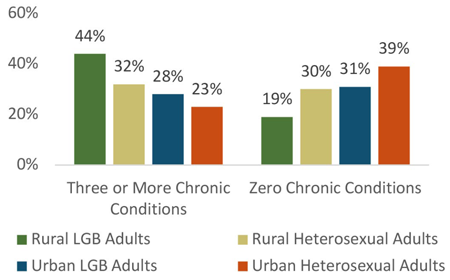
Among LGB adults, significant differences were found for arthritis (29.4% rural vs 14.7% urban), depression (54.0% rural vs 39.3% urban), diabetes (12.3% rural vs 4.8% urban), and hypertension (31.8% rural vs 20.8% urban).2
In both rural and urban settings, LGB adults, compared to heterosexual adults, had higher rates of asthma, depression, and anxiety disorder.2 However, heterosexual adults had higher rates of coronary heart disease and high cholesterol.2
Anxiety, Depression, and Access to Mental Health Care
When analyzing rural and urban LGB and heterosexual adults from 2019-2020, the highest levels of depression and anxiety disorder were found among rural LGB adults, with 38.6% reporting a dual diagnosis. Urban heterosexual adults had the highest rates of neither depression nor anxiety disorder diagnosis (81.0%).3 Additionally, among both rural and urban adults who felt depressed or took medication for depression, the severity of depression was higher for LGB adults.3 Rural LGB adults had the highest levels of depressed feelings, with 30.3% of those who had felt depressed saying the severity of depression was “a lot.”3
Prevalence of delaying mental health care was also affected by rurality and sexual orientation. Between rural adults with both a depression and anxiety disorder diagnosis, LGB adults were more likely than heterosexual adults to say they had delayed care because of cost (25.5% vs 13.9%).3 This delay of care was also higher for rural LGB adults with no depression or anxiety diagnosis, as compared to rural heterosexual adults with no diagnosis (9.9% vs 1.1%).3 See Figure 2.
Figure 2. Rural Adults Delaying Mental Health Care by Sexual Orientation, 2019-20203
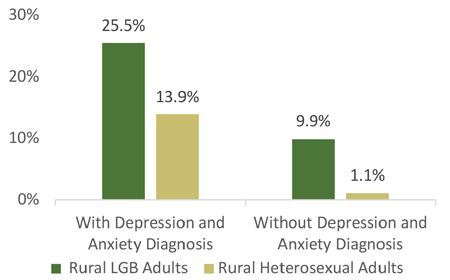
These inequities translated across urban respondents as well. Urban LGB adults were found to be less likely than urban heterosexual adults to have a usual source of care, regardless of depression or anxiety diagnoses.3 Urban LGB adults across all mental health diagnosis categories were also more likely to have delayed mental health care because of cost in the past 12 months, compared to urban heterosexual adults.3
Social Support for Transgender Individuals
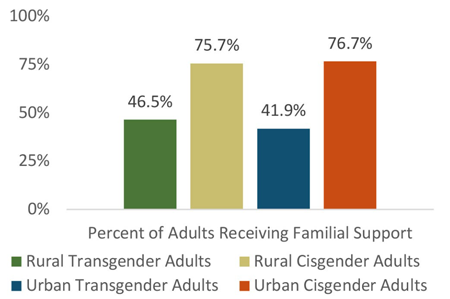
From 2016-2018, compared with rural cisgender adults, rural transgender adults were least likely to say they “very strongly” (7.0%) or “strongly” (9.3%) agree they get the social support they need from family members (vs. 32.3% and 29.1% of rural cisgender adults).4 Transgender adults, regardless of location, were less likely to agree that they received the social support they need compared to their cisgender counterparts (42.6% vs 76.6%).4 Rural transgender adults were also more likely to disagree that they get the familial support they need, compared to rural cisgender adults (40.8% vs 17.5%).4 This finding was similar in urban communities, with 47.3% of urban transgender adults reporting they do not get familial social support needed, compared to 14.9% of urban cisgender adults.4 Figure 3 depicts the percentage of adults who indicated any level of agreement (mildly, agree, and very strongly) that they receive familial social support.
Figure 3. Receipt of Familial Social Support by Gender Identity and Rurality, 2016-20184
Social and Emotional Support During COVID-19
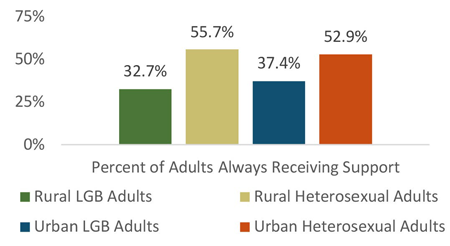
Data from 2020 showed that, among rural and urban LGB and heterosexual adults, rural LGB adults were the least likely to say that they always receive the social and emotional support that they need, while rural heterosexual adults were the most likely to say that they always receive that support (32.7% vs 55.7%).5 See Figure 4. When measured 12 months into the COVID-19 pandemic, rural LGB adults were the most likely to report receiving less social and emotional support compared to the year before the pandemic (23.5%).5 Urban LGB adults were the most likely to say they received more support than they had a year ago (22.9%).5
Figure 4. Receipt of Social and Emotional Support by Sexual Orientation and Rurality, 20205
Support Systems
A 2022 case study examined rural Pride celebrations and collected key informant perspectives to help identify positive community support systems and challenges faced by rural LGBTQ+ residents.6
Overarching themes showcased how Pride celebrations boosted rural LGBTQ+ individuals’, and the community's, well-being.6 These events also generally contribute positively toward participants’ mental health, especially for LGBTQ+ youth.6 These individuals commented on how they were able to interact with others like them in a positive environment, which was not always provided in other settings.6 Other attendees commented on overwhelming feelings of happiness and safety that accompanied Pride celebrations.6
Rural locations that hosted Pride celebrations also encountered challenges and difficulties in preparing for the event.6 Members of the community who opposed the celebration were often vocal about their opinions and would sometimes take action to try to hinder the progress of the event planning.6 These tactics would also affect members of the LBGTQ+ community in these areas, making them feel unwelcome.6 However, despite setbacks, some hosts feel that support for Pride celebrations is growing in their communities and feel optimistic for the future.6
Conclusion
When representatives from 14 LGBTQ+ support and advocacy organizations from around the U.S. were asked about challenges experienced by rural LGBTQ+ populations, the top two themes that emerged were lack of resources and lack of cultural competency.7 Lack of resources was related to limited financial and tangible resources to support LGBTQ+ individuals available in rural communities as compared to those available in urban areas.7 The theme of lacking cultural competency included concerns with health care providers who are not LGBTQ+ affirming, especially when caring for transgender individuals.7
Resources
- University of Minnesota Rural Health Research Center (2022). Self-Rated Health Among Gay, Lesbian, and Bisexual Adults: Rural/Urban Differences.
- University of Minnesota Rural Health Research Center (2022). Prevalence of Chronic Conditions by Sexual Orientation and Rural-Urban Location.
- University of Minnesota Rural Health Research Center (2022). Anxiety, Depression, and Access to Mental Health Care by Sexual Orientation and Rurality.
- University of Minnesota Rural Health Research Center (2023). Indicators of Familial Social Support by Rurality and Gender Identity.
- University of Minnesota Rural Health Research Center (2022). Social and Emotional Support During the COVID-19 Pandemic by Sexual Orientation and Rurality.
- University of Minnesota Rural Health Research Center (2022). Small-Town Pride Celebrations Supporting Social Connectedness & Well-Being for LGBTQ+ Rural Residents.
- University of Minnesota Rural Health Research Center (2022). Key Informant Perspectives on Supporting Health and Well-Being for LGBTQ+ Rural Residents.
