Opioid Use and Treatment Availability
January 2018
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration, the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. The RHRCs are committed to providing timely, quality national research on the most pressing rural health issues. This resource provides a summary of their most recent research on opioid use and treatment.
Opioid Use in Rural Communities
Opioids are prescribed for pain relief; most recognizable are morphine, hydrocodone, oxycodone, and fentanyl. Opioids also include the illegal drug, heroin. Opioid use disorder (OUD) (to include prescription drugs and heroin) is the fastest growing substance use problem in the nation.1 During 2008-13, 4.7% of U.S. residents ages 12 and older reported using non-medical opioids in the past year.1 Mean age at first use was 23.1 This did not vary between rural and urban communities.1 Among those who misused prescription opioids, 75% admitted to obtaining the pain relievers from someone who held a prescription for the drug.1 Despite implementation of treatment and prevention programs, rates of OUDs continue to rise in rural (non-metropolitan) and urban (metropolitan) communities alike (see Figure 1).1-2
Figure 1. Prevalence of Past-year Drug Use Disorders Over Time, by Geography2
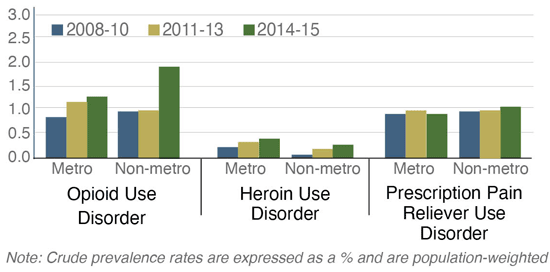
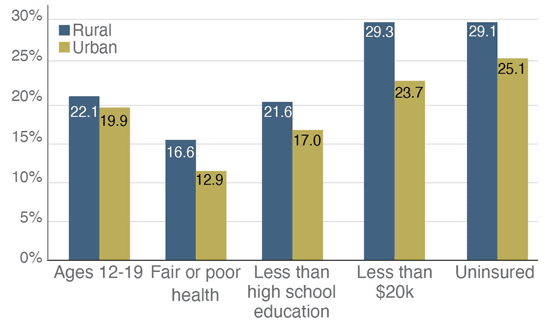
There has been little to no variation in the overall prevalence of OUDs between rural and urban populations. However, particular groups of rural residents have reported a greater prevalence of past-year use.1-2 Specifically, 8% of all rural residents ages 12-19 and 9.5% of those 20-29 had used opioids in the past year.1 Among those who had used opioids, rural were more likely than urban to be uninsured, low income, in poor health, and between ages 12-19 (see Figure 2).1
Rural opioid users were also more likely than urban to have ever been arrested (42.5% compared to 36.1%) and more likely to have been on probation in the past year (10.6% compared to 8.2%).1
Figure 2. Rural and Urban Opioid Users, 2008-131
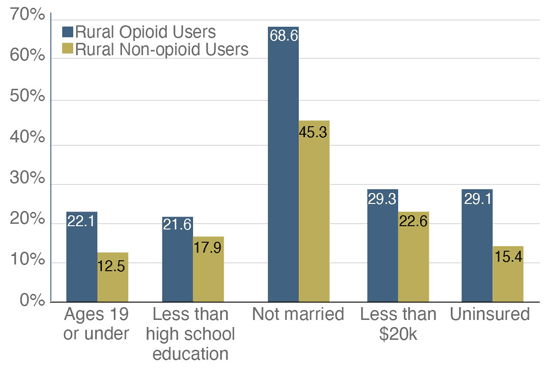
Among rural residents, those who had used opioids in the past year were more likely than those who had not used opioids to be under the age of 19, not married, low-income, and uninsured (see Figure 3).1
Figure 3. Rural Opioid and Non-opioid Users, 2008-131
Treatment for Opioid Use Disorder
Medication assisted treatment (MAT) is the use of medications in combination with counseling and behavioral therapies for the treatment of OUD. Buprenorphine-naloxone is one of the effective OUD treatment medications that may be provided in a primary care setting. The Drug Addiction Treatment Act (DATA) was passed in 2000 to expand OUD treatment options.3 DATA allows a physician to prescribe buprenorphine after he/she receives a waiver from the Drug Enforcement Agency (DEA).3 From 2012 through 2016, the percentage of counties with at least one waivered physician increased from 46.6% to 52.5%.3 However, while only 26.2% of urban counties were without a waivered provider in 2016, 60.1% of rural counties were still without one.3,4 The percentage of rural counties with a waivered provider has slightly increased since 2012; however, a majority of waivered providers (91.2%) are still disproportionately located in urban counties.3,4
Of the 1,124 rural physicians with DEA DATA waivers who were surveyed in 2016, only 60% were current prescribers accepting new patients.5 Overall, the most significant barriers of waivered prescribers providing MAT were diversion or misuse of medication (indicated by 48.4% of rural waivered providers), lack of available mental health support services (44.4%), and time constraints (40.2%).5 Non-prescribers (never and former prescribers) were significantly more likely than current prescribers to identify the following barriers: time constraints, lack of patient need, resistance from practice partners, lack of specialty backup for complex problems, lack of confidence in their ability to manage OUD, concerns about DEA intrusions on their practices, and attraction of drug users to their practices.5
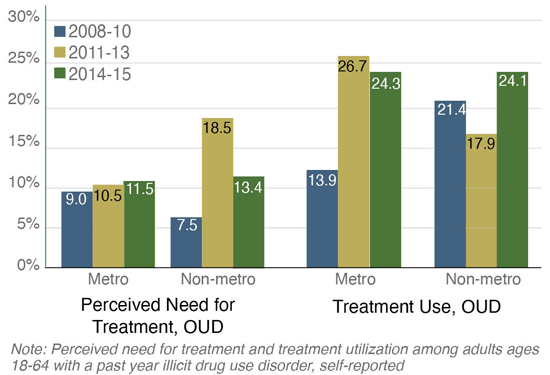
Perceived Need and Use of Treatment
Beyond the need for prescribers is concern with identified need for, and utilization of, treatment. The rate of perceived OUD treatment need among those with past year use did not vary significantly between rural (non-metro) and urban (metro) adults during 2014-15.6 However, the perceived need for treatment did increase significantly among rural users from 2008-10 to 2011-13.6 Most recently, treatment use for OUD did not vary between rural and urban adults, though rural adults reported a more significant increase in treatment from 2011-13 to 2014-15 (see Figure 4).6
Figure 4. Perceived Need for Treatment and Treatment Use Over Time for OUD, by Geography6
Rural Community Response
Rural community-based strategies are imperative for the prevention and treatment of and recovery from OUD and must expand beyond the availability of waivered prescribers. Specific rural challenges to the prevention/ treatment of OUD include workforce concerns, timely access to prevention and/or treatment, stigma, lack of community-provider collaborations, and providers not using current protocols for prescribing opioids.7 Community models for OUD treatment have included the use of telehealth, coalitions, evidenced-based prescribing protocols, emergency department protocols, and harm-reduction strategies through public health.7 Read, Rural Opioid Abuse Prevention and Treatment Strategies for more information on these programs.7
Resources
- Maine Rural Health Research Center (2016). Rural Opioid Abuse: Prevalence and User Characteristics.
- Rural and Underserved Health Research Center (2017). Illicit Drug Opioid Use Disorder Among Non-Metropolitan Residents.
- WWAMI Rural Health Research Center (2017). Changes in the Supply of Physicians With a DEA DATA Waiver to Prescribe Buprenorphine for Opioid Use Disorder.
- WWAMI Rural Health Research Center (2015). Geographic and Specialty Distribution of U.S. Physicians Trained to Treat Opioid Use Disorder.
- WWAMI Rural Health Research Center (2017). Barriers Rural Physicians Face Prescribing Buprenorphine for Opioid Use Disorder.
- Rural and Underserved Health Research Center (2017). Perceived Treatment Need and Treatment Utilization for Illicit Drug and Prescription Pain Reliever Use Disorders in Non-Metropolitan Areas.
- Maine Rural Health Research Center (2017). Rural Opioid Abuse Prevention and Treatment Strategies: The Experience in Four States.
