State of Rural Women's Healthcare Utilization and Health Indicators
April 2019
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. The RHRCs are committed to providing timely, quality research on the most pressing rural health issues. This resource provides a summary of some of their recent research.
Rural women face barriers to accessing preventive health screenings, mental health services, and maternal healthcare.1-3 Additionally, rural women report poorer health outcomes compared to their urban peers.1
Care Utilization and Health Indicators
Preventive health screenings are central to better health, yet rural women do not receive screenings at the same rate as women in urban areas. From 2014 to 2016:
- A significantly smaller proportion of rural women reported receiving a cholesterol check (67.8%) compared to urban women (71.7%).1
- Rural women ages 40-74 had significantly lower odds of receiving a mammogram in the past year compared to urban women in that age group.1
- Compared to urban women, rural women had significantly lower odds of ever being vaccinated against HPV.1
Greater proportions of women in rural communities also reported negative health indicators compared to women in urban areas.1 See Figure 1.
Figure 1: Women's Health Indicators, 2014-161
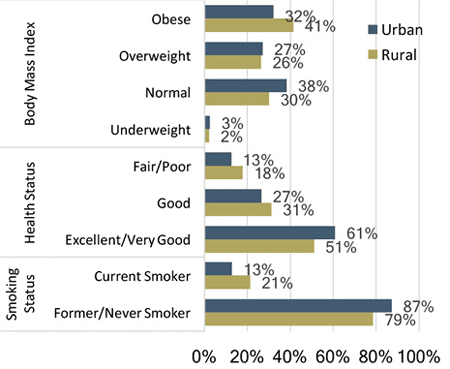
All residence differences significant at p < .001.
In examining use of the Emergency Department (ED) for Mental Health (MH) and Substance Abuse (SA) diagnoses, research found that 61% of all MH/SA visits were for women.2 Women used the ED for MH diagnoses at a much higher rate than for SA; these visits were predominantly diagnosed as anxiety or mood disorder.2 Results were consistent across urban, large rural, small rural, and isolated rural areas.2
Rural Maternal Healthcare
Rural women lack access to maternal and obstetric healthcare services. As of 2014:
- 54% of rural counties lacked hospital-based obstetric (OB) services (up from 45% in 2004).4
- Only 30.2% of rural noncore counties had in-county, hospital-based OB care compared to 77.9% of micropolitan counties.4
- 78% of rural counties in Florida reported no in-county hospital OB services compared to only 9% of rural counties in Vermont, indicating significant variability by state.5
Read Rural Obstetric Services: Access, Workforce, and Impact for more information. Rural hospital and OB unit closures require pregnant women to find alternative care providers or health systems; these women identify travel as a significant barrier to care.3 Similarly, women in less densely populated rural areas were more likely to give birth in a non-local hospital (35.97%) than those living in micropolitan areas (20%) indicating lack of local access and increased travel time and distance.6
A 2017 focus group comprised of rural pregnant women living in an area with a seasonal pattern of work dependent on tourism indicated additional barriers to quality maternal health.
Barriers to care included:
- Community support/flexibility of their work schedule
- Pressure to time pregnancy outside of the busy season
- Taking the time needed to make appointments
- Little breastfeeding support
- Limited childcare options7
Between 2002 and 2010, both rural and urban hospitals saw rates of low-risk and nonindicated cesarean deliveries increase and vaginal birth after cesarean (VBAC) rates decrease.8 Rural hospitals had a lower rate of nonindicated labor induction in 2002 but that rate sharply increased by 2010.8 High birth volume hospitals had lower odds of low-risk (14.67%) and nonindicated cesarean (16%) compared to low volume hospitals (16.1% and 17% respectively).9
Rural Maternal Substance Use
According to data from 2008 through 2013, rural mothers (women with children under the age of 18 living in the home) were significantly more likely to smoke than urban mothers.10 Specifically:
- 38.7% of rural mothers reported past-year smoking compared to 24% of urban mothers.
- 26% indicated past-month daily smoking compared to 12.4% of urban mothers.
- 10.6% of rural mothers identified smoking heavily compared to only 4% of urban mothers.10
Nearly half (48.8%) of rural single mothers reported smoking in the past month compared to 33.5% of urban single mothers.10
Rates of opioid use disorder (OUD) among pregnant women and rates of neonatal abstinence syndrome (NAS) have continued to increase.11 In data from 2007 to 2014, these conditions were more prevalent among rural pregnant women who gave birth/babies who were born in urban teaching hospitals.11 See Figure 2. Prevalence of NAS was higher than OUD, suggesting that healthcare professionals are missing OUD diagnoses or mothers are using opioids for medical reasons which would not constitute an OUD diagnosis.11
Figure 2: Prevalence of Maternal OUD and Infant NAS Among Rural Women by Hospital Type11
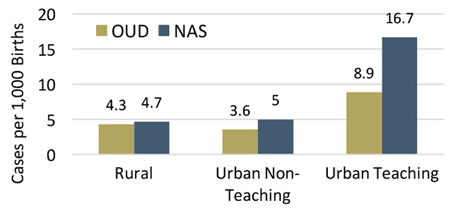
Having a high school education or less increased odds of opioid use among rural pregnant women.12 Other substance use and diagnosis of anxiety or depression increased odds of opioid use for urban and rural pregnant women.12 Though not statistically significant, 6.7% of rural women reported non-medical opioid use compared to 5% of urban.12
Conclusion
A greater proportion of rural women compared to urban identified as obese and as current smokers. They reported substance use while pregnant and indicated worse overall health status and lower preventive screening rates. Communities and healthcare policy must focus on increasing access to quality healthcare for rural women, including nutrition programs, OB services, tobacco cessation programs, and other preventive health services.
Resources
- Maine Rural Health Research Center (2019). Preventive Health Service Use Among Rural Women.
- North Dakota and NORC Rural Health Reform Policy Research Center (2017). Use of the Emergency Department for Mental Health and Substance Abuse Among Women.
- University of Minnesota Rural Health Research Center (2016). Ensuring Access to High-Quality Maternity Care in Rural America.
- University of Minnesota Rural Health Research Center (2017). Closure of Hospital Obstetric Services Disproportionately Affects Less-Populated Counties.
- University of Minnesota Rural Health Research Center (2017). State Variability in Access to Hospital-Based Obstetric Services in Rural US Counties.
- University of Minnesota Rural Health Research Center (2015). Rural Women Delivering Babies in Non-Local Hospitals: Differences by Rurality and Insurance Status.
- University of Minnesota Rural Health Research Center (2018). Challenges Related to Pregnancy and Returning to Work after Childbirth in a Rural, Tourism-Dependent Community.
- University of Minnesota Rural Health Research Center (2014). Rural-Urban Differences in Obstetric Care 2002-2010 and Implications for the Future.
- University of Minnesota Rural Health Research Center (2014). Birth Volume and the Quality of Care in Rural Hospitals.
- Maine Rural Health Research Center (2015). Implications of Rural Residence and Single Mother Status for Maternal Smoking Behaviors.
- University of Minnesota Rural Health Research Center (2018). Practical Implications: Opioid-Affected Births to Rural Residents.
- University of Minnesota Rural Health Research Center (2018). Non-Medical Opioid Use Among Rural and Urban Pregnant Women 2007-2014.
